HEALTH ALERT
In what the Los
Angeles Times is referring to as a meningitis
outbreak in L.A.'s gay community, since January 1 there have been
eight occurrences of invasive meningococcal disease in L.A. County. Four of
those cases have been of gay men, and three
of those four have died, officials reported Thursday.
http://www.breitbart.com/Big-Government/2014/04/03/Meningitis-Outbreak-In-LA-Gay-Community-Three-Dead
* Special thanks to "Google Images",
"LA Weekly", "Los Angeles Times", "CNN",
and "ntheknowpeel.ca/stiaids/list.htm."
and "ntheknowpeel.ca/stiaids/list.htm."
BLOG POST
by Felicity Blaze Noodleman
Los Angeles, CA
5. 9.14
A few weeks ago an article appeared in the "LA Weekly" which was beyond belief. It's very hard to write about a subject that makes you so scared and angry, a subject which shakes you to the very core of your being, especially when this problem is so preventable. It is a subject which is a threat to your health and well being but we will try to get a grip on the problem and write as objectively about the issues.
Public health officials are seeing a rise in cases of Meningitis and Syphilis in Gay Communities across the US and not just in LA and San Francisco but in NYC and Miami - in fact all large city's in the country could be effected. We are not experts in the field of health care but we do want to alert our readers about the problem. As usual we are posting our information and sources.
It is not surprising that since the AIDS became the number one health issue in the gay community that other diseases would soon follow since the AIDS disease attacks the immune system and the body's ability to fight off other diseases. STD'S (sexually transmitted diseases) seem to be logical considering the free and unprotected sexual life styles of many gay men. In short; this phenomenon is not really a surprise.
The one big question which still remains is how do we deal with the problems arising from the irresponsible sexual behavior of the gay life style? There are no creative solutions and few medical treatments for AIDS. The best advice for us all is to practice safe sex and avoid the pitfalls and snares of the gay life style. It's just that simple. Other wise your life could turn into a nightmare of the worst sort.
We are running very few photographic illustrations for most of this article. Many of these STD'S would be considered too disturbing for some readers. These photos may be found at wikipedia.com or by Googling Syphilis.
It is not surprising that since the AIDS became the number one health issue in the gay community that other diseases would soon follow since the AIDS disease attacks the immune system and the body's ability to fight off other diseases. STD'S (sexually transmitted diseases) seem to be logical considering the free and unprotected sexual life styles of many gay men. In short; this phenomenon is not really a surprise.
The one big question which still remains is how do we deal with the problems arising from the irresponsible sexual behavior of the gay life style? There are no creative solutions and few medical treatments for AIDS. The best advice for us all is to practice safe sex and avoid the pitfalls and snares of the gay life style. It's just that simple. Other wise your life could turn into a nightmare of the worst sort.
We are running very few photographic illustrations for most of this article. Many of these STD'S would be considered too disturbing for some readers. These photos may be found at wikipedia.com or by Googling Syphilis.
Tell me more about bacterial
meningitis.
Meningitis is
an infection of the spinal fluid and of the membranes surrounding the brain
(the meninges). Before the Hib vaccine was approved for use, Haemophilus
influenzae B
was the most common cause of meningitis. Now, however, most cases of meningitis
are caused by Streptococcus pneumoniae or Neisseria
meningitidis.
Bacterial meningitis is a very serious
disease, with a 10-15% mortality rate, and 10-15% of those who survive have
permanent damage, including hearing loss, loss of limbs, and mental
retardation.
How is bacterial meningitis
transmitted?
Although epidemics of meningitis do
occur, mainly in the "meningitis belt" of central Africa, bacterial
meningitis is mainly transmitted by carriers of either S.
pneumoniae or N.
meningitidis, via
direct contact with their respiratory secretions.
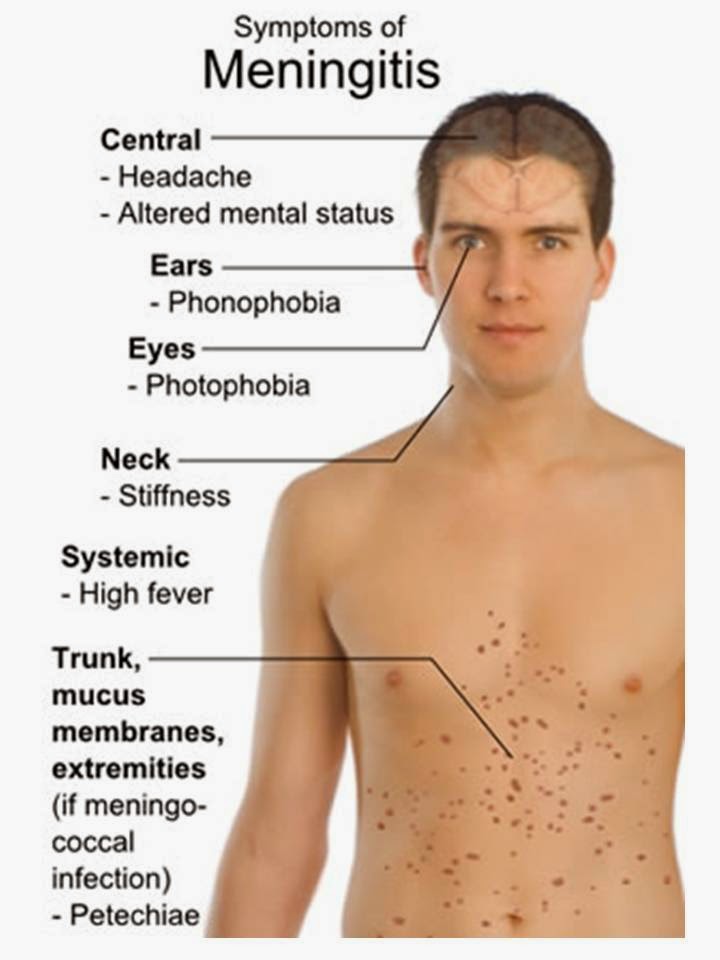
What are the symptoms of bacterial
meningitis?
The symptoms of meningitis are the same
regardless of the cause: fever, headache, and stiff neck. As the disease
advances, a rash may appear on the infected person, which are spots of dead
tissue, destroyed by the invading bacteria.
Meningitis is an extremely fast-moving
infection- there have been cases of people feeling perfectly healthy in the
morning and dead by nightfall. Should the above symptoms appear, it is crucial
that you seek medical attention immediately.
Because the symptoms of meningitis are
identical regardless of whether the infection is caused by a virus or by
bacteria, a laboratory diagnosis is crucial to treatment. In the case of a
bacterial infection, laboratory tests will also determine the species and type
of infecting bacteria so that the right antibiotics can be used.
How is bacterial meningitis
treated?
Bacterial meningitis essentially requires
hospitalization so that symptoms can be monitored, and so that large doses of
antibiotics can be given intravenously. Prompt, appropriate antibiotic therapy
can reduce the risk of dying from bacterial meningitis to around 15%.
How can I prevent meningitis?
Vaccines exist against all different
types of bacterial meningitis. Vaccines against S. pneumoniae and
H. influenzae B (Hib) are
part of the recommended childhood vaccination series. A new vaccine against N. meningitidis has
just been approved for older children and adolescents, who have a very high
rate of bacterial meningitis. It is also recommended for college freshman
living in dorms, who are three times more likely than other persons their age
to contract meningitis.
http://www.co.monroe.mi.us/government/departments_offices/public_health/bacterial_meningitis.html
“The Los Angeles Times”
Deadly
L.A.- Area Meningitis Cases Raise Concerns In Gay Community
April
04, 2014
By Hailey Branson-Potts
As
three people were confirmed dead this week after having contracted meningitis
in Los Angeles County, at least one medical expert said there is a
"pretty strong signal" that men who have sex with men are at
increased risk for the rare bacterial infection.
Robert
Bolan, the medical director at the L.A. Gay & Lesbian Center, said there is
cause for concern in the gay community because the infection rate is higher in
men who have sex with men and especially higher in those who are HIV-positive.
Bolan
said it is unclear why the disease seems to affect men who have sex with men at
a higher rate, though the weakened immune systems of people who are
HIV-positive might make them more susceptible.
“I
think the important thing to understand is this is not an epidemic,” Bolan
said. “But there’s a pretty strong signal that men who have sex with men, at
least those who are HIV-positive, are at increased risk for invasive
meningococcal disease.”
The
county health department announced earlier this week that there have been
eight cases of invasive meningococcal disease in the county so far this year.
Four cases occurred in men who have sex with men, and three of those involved men who were
HIV-positive, county health officials said. On Thursday, officials said three
of them had died. The victims were 27 or 28.
Some
of those sickened lived or socialized in West Hollywood and North Hollywood,
officials said.
The
deaths come less than a year after L.A. gay’s community grappled with another meningitis
scare.
Brett
Shaad, a 33-year-old West Hollywood resident and attorney, contracted
meningitis in April 2013 after attending a gathering of gay men in Palm
Springs. He died days later.
The
AIDS Healthcare Foundation responded by offering free meningitis vaccines.
County health officials eventually offered the vaccine for low-income and
uninsured residents.
This
time around, the county is providing free vaccinations for patients without
health insurance.
Invasive
meningococcal disease stems from a rare bacterial infection
that can spread to the blood, brain or spinal cord and can affect the entire
body -- sometimes causing death.
It
is spread by close exposure to sneezing or coughing or direct contact with
saliva or nose mucus -- though it's less contagious than influenza, the county health department said.
Activities
associated with risk for the illness include smoking, close contact with an
infected person such as kissing or sharing beverages or cigarettes, and living
in group settings for prolonged periods.
Symptoms
of the illness usually strike within five days of exposure to the bacteria, and
may include a high fever, stiff neck, aversion to bright light and aches.
Those
interested in the free vaccinations can call 211 or visit the department's website to get a
listing of provider clinics.
“The Los Angeles Times”
By Mikael Häggström, via Wikimedia Commons
http://www.news-medical.net/health/Meningitis-Symptoms.aspx
Syphilis Classification and external
resources Electron
micrograph of Treponema pallidum.
http://en.wikipedia.org/wiki/Syphilis
Gay Syphilis
Scourge Skyrockets
County officials dawdle, leisurely
launching another questionable ad campaign
by Patrick Range McDonald
Wednesday,
Jul 11 2007
FIVE
YEARS AGO, the honchos at the Los Angeles
County Department of Public Health were caught off guard. An outbreak of
syphilis among gay men suddenly popped up on their radar, and leaders in the
gay community quickly put pressure on the health officials to launch a timely
marketing campaign to warn the public.
They
chose a mascot for the county’s marketing campaign — a cartoon drawing of an
unidentifiable red blob named Phil, meant to represent a syphilis sore. But in
a decision that set the wags talking about absurd Los Angeles prudishness,
county officials refused to also use a smiling cartoon of a talking “healthy
penis” — a drawing so inoffensive it looked like a bratwurst.
San
Francisco and Seattle used both the penis and the Phil cartoon in their
campaigns, but Los Angeles officials, located in the filming capital of tits
and ass, couldn’t handle the image of a happy cock. “The county was more
concerned about people’s tender sensibilities than getting the message out,”
says Michael Weinstein, president of AIDS Healthcare Foundation, the nation’s
largest provider of HIV/AIDS medical care.
Today,
the Department of Public Health faces a much bigger problem than that old
dustup: That syphilis outbreak has not only refused to go away, but infection
rates among gay and bisexual men have skyrocketed 365 percent between 2001 ?and
2005 to 1,585 cases.
The
bad news gets worse. On June 29, the federal Centers for Disease Control and
Prevention announced that neurosyphilis — a serious and rare form of syphilis,
which can lead to blindness and stroke — had been found in HIV-positive gay and
bisexual men in Los Angeles, San Diego, Chicago and New York.
Yet,
in what appears to be a replay of their timidity five years ago, county
bureaucrats have been extremely slow to react, failing to beef up their
traditional three-pronged attack using prevention, testing and education — a
proven strategy for fighting the syphilis scourge in other cities.
Critics
are peeved that government bureaucrats in Los Angeles County, despite the
raging syphilis and emergent neurosyphilis in gay men, have leisurely spent
their time over the past year developing and testing yet another marketing
campaign.
“Public
Health almost promotes bad health as they keep fiddling and we keep telling
them it’s going to get worse and worse,” says Miki Jackson, an activist and
health care consultant to the gay and lesbian community. “And we’ve been right
more times than we would like.”
Organizations
such as AIDS Healthcare Foundation, AIDS Project Los Angeles and the Los
Angeles Gay and Lesbian Center have been warning county health officials
including Dr. Jonathan Fielding, director of Public Health, and John Schunhoff,
chief of operations of Public Health, for years.
WHAT’S
REALLY TROUBLING, critics say, is that while these
leaders at Public Health knew something was going awry in their fight against
syphilis, they moved aggravatingly slowly. In 2000, cases of syphilis among gay
men zoomed from zero to 69, but after running an outreach program for just two
months, the county declared success and stopped funding it. Gay leaders were
mystified, warning health officials that the situation was worsening — and in
2001 syphilis cases jumped to 85.
In
recent months, with the new numbers showing a massive problem, county officials
argue that they didn’t issue a call for more action because the sharply rising
data simply reflected the fact that more people who harbored syphilis had
decided to be screened. “If you’re successful in getting people tested,” explains
Schunhoff, “the numbers go up.”
On
one level, Schunhoff’s right. But even he was reluctant to explain away the
spike merely as a surge in data. In 2005, the county stopped funding the widely
seen campaign using Phil the syphilis sore — the year syphilis infections hit a
peak of 1,585 cases. And until last week, the county, with its $19.38 billion
budget, had failed for 18 months to fund any public-education campaign warning
of the mounting syphilis scourge.
“With
HIV/AIDS, the county has been pretty responsive,” says Whitney Engeran III,
director of prevention and testing at AIDS Healthcare Foundation. “When it
comes to [sexually transmitted diseases], however, there’s not the same kind of
action.”
Critics
say the dichotomy is mind-boggling, since rising rates of sexually transmitted
diseases clearly signal an increase in unsafe sex practices. And unsafe sex
leads to more HIV/AIDS cases. Moreover, experts in Los Angeles point out that
men with syphilis sores are more susceptible to HIV/AIDS. Either way, syphilis
and other spreading diseases are not simply the material for crude jokes
anymore. In the long run, they spell big trouble.
Schunhoff
defends the 18 months it took the lumbering county to create its brand-new
marketing campaign, featuring a hunky, half-naked man wrapped in a white towel
preparing to take a shower, with the slogan: “Check yourself. Don’t assume
you’re getting off clean.”
“We
were trying to get a campaign that works with focus groups,” Schunhoff says.
“The [Los Angeles County] Board of Supervisors wanted something that was really
effective.” He predicts optimistically, “I think the outcome will result with
more testing.”
Yet
county officials never asked the gay health care community, with its decades of
marketing experience, what “effectiveness” looks like, according to Miki
Jackson. “They kept the entire campaign a secret,” she charges. “We had no
input, and whenever we asked them a question, they were silent about it.”
AS
DISCONNECTED as Fieldingis from these gay health
care experts, however, he should still only take so much heat for a problem
clearly caused by gay and bisexual men who insist on having sex without
condoms.
Jackson
points to a deadly silence within the community. She believes this widespread
silence causes outbreaks like syphilis. “People don’t want to talk about AIDS
or syphilis. It brings up the past and bad memories. They’re in great denial.”
Craig
Thompson, executive director of AIDS Project Los Angeles, similarly blames
“condom fatigue” — an attitude harbored by young men who weren’t around when
AIDS was a virtual death sentence, as well as denial among men who even now
aren’t comfortable with their homosexuality.
“The
more homosexuality is hidden,” says Thompson, “the less likely you are going to
negotiate safe sex.”
West
Hollywood Mayor John Duran sees the use of crystal meth as a major culprit in
the ballooning syphilis scourge. “It grabs people right from the very start,
and people become addicted very quickly,” says Duran. “So they don’t have the
ability to make the right choices.”
Duran
also believes, “The message wears down after hearing this stuff for 20 years.
We have to come up with something new.” Duran expects to start up a gay men’s
health forum.
But
for Michael Weinstein of AIDS Healthcare, the issue is more clear cut: “There
has been a decline of safer sex in the gay community, and there hasn’t been a
call to arms about it.”
Weinstein
is a rare voice in Los Angeles, consistently and loudly demanding personal
responsibility when it comes to gay sex. Only a few years ago, posters
featuring a photograph of Weinstein mysteriously appeared in the windows of
West Hollywood bars on Santa Monica Boulevard, labeling Weinstein a “Condom
Nazi.”
At
the time, Weinstein was pushing a citywide public referendum for mandatory
condom distribution at all West Hollywood bars and clubs. The voters in the
35,716-resident city, which is about 40 percent gay or bisexual, shot him down,
and Weinstein was shocked that people turned against him.
“There
are people in the gay community who say we shouldn’t hold people responsible,”
Weinstein says, “and they are very militant about it.”
Regardless,
the stubborn Weinstein has a plan to create a social climate where unsafe sex
is not tolerated. Just as “friends don’t let friends drive drunk,” Weinstein
wants gay men to accept the same notion about safe sex.
“Men
— gay or straight — don’t want to use condoms,” he says, “but that doesn’t mean
you can’t succeed.” Toward that end, AIDS Healthcare’s own marketing campaign
emphasizes that testing and prevention should be a part of one’s grooming
routine, like working out at the gym or brushing your teeth.
“It
doesn’t help to judge,” says Weinstein, “but you can get the information out
there and encourage people to get tested.”
In
the meantime, bureaucrats at the county’s sprawling Department of Public Health
will, in their own words, fight syphilis with “guerrilla marketing tactics” —
and probably cross their fingers. Their new outreach program will run for two
years. But if history repeats itself, they may need to start working on a
replacement campaign today.?
“LA Weekly”
Symptoms for syphilis are harder to detect in women during the early stages of the disease. This posters acknowledges the social
stigma of syphilis, while urging those who possibly have the disease to be
tested. (circa
1936)
http://en.wikipedia.org/wiki/Syphilis
"CNN"
The above image was published in
LIFE Magazine in November 1990 showing AIDS patient David Kirby taking his last
breaths surrounded by his family in Ohio. The image, shot by Therese Frare,
became the face of the HIV/AIDS epidemic. See the entire collection of images
on Life.com.
http://www.cnn.com/2014/05/07/opinion/cole-sidibe-aids-research/
How To Find An AIDS Cure For All
By Kenneth Cole and Michel
Sidibé
updated 8:48 AM EDT, Wed May 7, 2014
(CNN) -- Thirty years ago around this
time of the year, scientists announced that the probable cause of AIDS had been found.
Human immunodeficiency virus, or HIV, would subsequently enter our lexicon and become
synonymous -- no matter where you lived -- with death. Since then, more than 75 million people have acquired
HIV and nearly 35.6 million have died of AIDS-related illnesses.
With no cure in sight, it seemed that ending this epidemic would be a Sisyphean
task.
But
investments in AIDS research, prevention and treatment have yielded tremendous
dividends. As a result, we have before us the opportunity to end one of the
greatest public health crises in history.
More
people than ever are receiving life-saving antiretroviral therapy, and are
living healthier, longer lives. There have been historic declines in AIDS-related
deaths worldwide. From 1996 to 2012, antiretroviral therapy averted 6.6 million
AIDS-related deaths, including 5.5 million in developing countries. The annual
number of new HIV infections has also dropped by 33% since 2001. In 26
countries, the rate of new HIV infections among young people (ages 15-24)
decreased by 50% since 2001. For the first time, we have the ability to end the
transmission from mother to child and to keep mothers alive.
Merely
a decade ago, few believed they would see a cure in their lifetimes. However,
several people who have been cured have helped shine a light on how a cure for
all could be found. The case of a Berlin patient, the first person to be cured
of HIV, was reported in 2008 and represented a watershed
moment in HIV research and a proof of principle that a cure was possible. Last
year, researchers documented the case of the first child to be functionally
cured of HIV.
Yet
despite these promising developments, the epidemic is far from over. We are one
year away from the target date for achieving universal access to HIV
prevention, treatment and care set forth in the United Nations 2011 Political
Declaration on AIDS, and we have a lot of work to do to meet that goal. Of the
35.3 million people living with HIV, nearly two out of three living in
developing countries are not on HIV treatment, either because they do not have
access or do not know their HIV status.
Scaling
up access to HIV treatment remains an essential prerequisite for ending AIDS.
In addition to saving lives, it has proven to be highly effective at preventing
HIV transmission because treatment reduces the chance the virus can
spread by 96%. We must also improve our health systems to support
the scale-up of core interventions that we know work, including expanded access
to HIV prevention and treatment, prevention of mother-to-child transmission of
HIV, harm reduction, and voluntary medical male circumcision.
Effective
outreach to those most at risk—and most in need—is also critical. Key
populations, including sex workers, men who have sex with men, transgender
individuals, people who inject drugs, young girls and women often face
substantial barriers to obtaining prevention, treatment and care services. As a
result, efforts to reduce HIV transmission among vulnerable populations remain
insufficient.
Moving
forward, research on a cure and vaccine remains essential and must be a
priority. The quest for a safe and effective vaccine to prevent HIV has seen
hopeful signs of progress. Recently, an experimental vaccine "cleared" HIV in
monkeys infected with the virus. Broadly neutralizing antibodies
that protect against a wide range of strains of HIV have been discovered.
Experts are following up the RV144 trial in Thailand, the first vaccine to show
a modest protective effect in humans, in order to understand why some people
were more protected than others and how to make the protective effect last
longer.
HIV
cure research has gained momentum and picked up speed. The first organization
to aggressively pursue cure-focused HIV research, amfAR, The Foundation for
AIDS Research, has intensified its cure research program and set a goal to find
a broadly applicable cure for HIV by 2020 with its "Countdown to a Cure
for AIDS" initiative.
The
foundation plans to invest $100 million in cure research over the next six
years. And on World AIDS Day last December, President Obama announced $100
million in reprioritized funding over the next three years to launch a new HIV
Cure Initiative at the National Institutes of Health. The scientific obstacles
to a cure have been illuminated, and with a vigorous research effort and
sufficient investment, these challenges can be overcome.
While
we now have the tools to begin to end the HIV epidemic, achieving an AIDS-free
generation is threatened by a considerable gap between available resources and
the amounts needed to scale up high-impact interventions. Investing now in
these interventions will not only accelerate progress in reducing AIDS-related
deaths and new HIV infections, but it will also lower the long-term cost of the
HIV response. Strong, continuous U.S. leadership at this critical moment is
key.
Innovative
financing options and strategies need to be explored to ensure that the global
HIV response is sustained. UNAIDS supports many countries in developing HIV
investment cases, which enable countries to estimate future resource gaps,
identify new sources of domestic financing to help close the gaps, and agree on
ways to enhance the efficiency and impact of spending. More than 30 countries
are now planning to develop their own investment cases by the end of this year.
Lastly,
we must eliminate stigma, discrimination and punitive laws and practices that
continue to undermine efforts to provide critical services to prevent and treat
HIV, especially among vulnerable populations. We're seeing a growing
conservatism in a growing number of regions and countries.
State-sanctioned
homophobia in many countries remains a formidable barrier to the implementation
and uptake of HIV programs. More than 80 countries criminalize
homosexual behavior. The anti-homosexuality laws that have gone into effect in
India, Nigeria, Russia and Uganda, for example, could impede their national
responses to HIV. Studies have clearly shown that criminalizing same-sex sexual
behavior poses an immense structural barrier to HIV prevention.
We
all are stakeholders in the opportunity before us now. Addressing the
unfinished business of ending the pandemic will require the cooperation and
full commitment of national government leadership, scientists, civil society,
and people living with HIV. But through continued and strengthened solidarity,
we will be able to rise above the challenges that remain ahead to ultimately
achieve the goal of an AIDS-free generation.
We would like to provide a list of STD'S and STI'S to fully inform you of the dangers to be mindful of which has been provided by http://intheknowpeel.ca/stiaids/list.htm. Many of these are treatable. If you suspect you may be at risk see your doctor immediately or if expense is a problem see a County Free Clinic. They want to see you as soon as possible!
Disclaimer
• Routine
screen—all individuals reported to be engaging in sexual activity that may put
them at risk are offered STI testing
• Repeat
testing may be required based on clinical assessment
STIs
• Bacterial Vaginosis
• Chlamydia
• Genital Herpes
• Gonorrhea
• Hepatitis B
• Hepatitis C
• Human Papillomavirus
• Lymphogranuloma Venereum (LGV)
• Pubic Lice (Crabs)
• Scabies
• Syphilis
• Trichomoniasis
• Yeast Infections
If you think you might have a sexually
transmitted infection, get it checked out as soon as possible. You can see your
family doctor or visit a Healthy Sexuality Clinic in your area to find
out exactly what you have and how you can treat it. And to be on the safe side,
it's best to avoid having sex until you've seen a doctor about your concerns.
This has been Felicity working for you. See you next week!
Tell your friends and associates about us!
It's easy! Just copy and paste me into your
email!
The Noodleman Group is on Google "Blogger"!









No comments:
Post a Comment